
When timely alerts can help save lives
Babysense is a highly sensitive non-touch baby Breathing Movement Monitor. Now parents can get the peace of mind while their baby sleeps. Babysense is intended for detection of respiratory cessation (apnea) in babies. It constantly monitors baby’s breathing micro movements through the mattress during sleep and gives an alert to caretakers if breathing stops or becomes irregularly slow, giving critical time to intervene. A quick response can make the difference between something minor and a critical situation.
Babysense is the original world’s first Breathing Movement Monitor in its kind. All derivations which are available today on the market are a result of this breakthrough in development.
Babysense was developed in view of the dangers that infants may face in hospitals and at homes associated with sudden infant death syndrome (commonly known as SIDS and Cot or Crib Death). SIDS remains a significant cause of death among basically healthy infants up to one year of age, with an average death toll reaching circa 22,000 babies per year worldwide.
Babysense breathing movement monitor is highly effective and has helped protecting over 1 million babies from SIDS around the world. Babysense is a vital measure of protection, which, when combined with safe sleeping precautions provides safety and peace of mind.
Babysense is a registered class IIb medical device, approved to the Medical Devices Directive (CE) 93/42/EEC. It is clinically tested and field proven in hospitals, parents and healthcare providers with enhanced means to cope with threats associated with SIDS.
Technology that provides continuous protection at all times
Babysense technology along with its highly sensitive sensor pads allow monitoring and detecting even the slightest breathing movements through the mattress.
Babysense is more than just a commonly known MOVEMENT MONITOR!!! Babysense breathing movement monitor alerts caregivers about a potential threat before it strikes and not only after the baby stopped breathing.
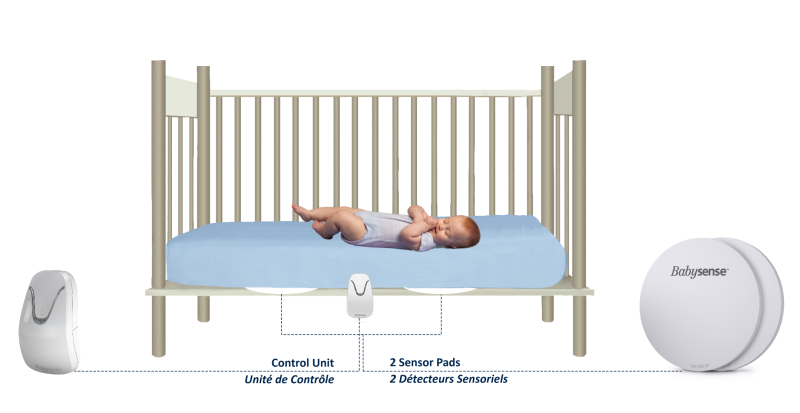
The control unit is connected to Babysense sensor pads placed between infant’s mattress and crib or bed base.
Babysense monitors operate on regular AA batteries, so there are no dangerous power cords. Babysense 7 features a new “Hidden Cable Installation” concept. The passive sensor system is totally safe and has no direct contact with the baby.
Babysense breathing movement monitor identifies your baby’s respiratory patterns which are transmitted to a compact microprocessor, in the Babysense control unit, where they trigger a flashing green light that is clearly visible from a distance. The flashing green light is the signal that all is well, providing a parent or caretaker peace of mind.
If, for whatever reason, no breathing is detected within 20 seconds, or if the breath rate slows to less than 10 breaths per minute, a red LED light will illuminate and an audible alarm will sound. On hearing this alarm, a parent or caretaker is alerted to come to the aid of the sleeping baby.
- Modern, compact and easy to use design with single button operation
- Improved Sensitivity Concept – Lower risk of false alarms
- Medically certified and clinically proven technology with more than 25 years of global experience
- Totally safe and emits no radiation of any kind that may harm the baby
- Auditory and visual (red light) alarm is activated if breathing stops or becomes irregularly slow
- Two highly sensitive sensor pads cover the entire crib area and do not come into contact with the baby
- Operates on regular household batteries – no exposed cords, no connection to mains
- Suitable for all basically healthy babies from birth up to one year of age
- Safe, hack-proof technology with no interference from other electronic household devices
Clinical Trial
Babysense is clinically proven to be accurate in detecting breathing irregularities and cessations
Purpose: To study the accuracy of a movement sensor placed under the mattress in alarming for apnea and bradycardia in infants.
Conclusions: Under the mattress movement sensing is accurate in alarming for apnea and bradycardia in infants. Since the usage of this system is simple and without direct contact with the infant, it may be a convenient useful method for certain infants.
What Medical Professionals have to say
What our customers are saying


Under-the-mattress movement sensor (Babysense*) versus
cardiorespiratory monitor to alarm in apnea of infancy
Mordechai O1, Shehadeh N1, Pillar G1,2
1 Pediatrics Department, Rambam Medical Center and Technion Faculty of Medicine, Haifa
2 Pediatrics Department, Carmel Hospital and Technion Faculty of Medicine, Haifa, ISRAEL
Abstract
Background: Infant home monitors are recommended in high risk infants. While direct monitoring of respiration and heart rate requires attaching surface electrodes to the infant, movement sensors may be placed under the mattress and detect respiratory cessations without
touching the infant.
Purpose: To study the accuracy of a movement sensor placed under the mattress in alarming for apnea and bradycardia in infants.
Methods: 54 high risk infants who presented to the emergency room with Apparent Life Threatening Event (ALTE) underwent a whole night simultaneous monitoring by both cardiorespiratory monitor (intellivue MP20 junior, Phillips) and under the mattress movement monitor (Babysense II, Hisense). The cardiorespiratory monitor was set to alarm when detecting no respiration for 20sec, heart rate below 90/min, and oxygen saturation below 90%. The Babysense was set to alarm when detecting no respiration (movement) for 20sec.
Results: 54 infants (age 47±40 days) who presented to Rambam (n=49) or Carmel (n=5) emergency rooms after ALTE participated. During 80 nights of monitoring (18 infants were monitored for 2 nights, 4 infants were monitored for 3 nights) there were 8 events of alarming
(10%), simultaneously in both systems. In all other cases there were no alarms in both systems.
Conclusions: Under the mattress movement sensing is accurate in alarming for apnea and bradycardia in infants. Since the usage of this system is simple and without direct contact with the infant, it may be a convenient useful method for certain infants.
Introduction
Sudden infant death syndrome (SIDS) is defined as the sudden death of an infant younger than one year of age, which remains unexplained after a thorough case investigation, including performance of a complete autopsy, examination of the death scene, and review of the
clinical history. It is considered as the most prevalent cause of infant deaths between the ages of 1 month and 1 year (1). The prevalence of SIDS has substantially decreased in recent years in the developed world and in Israel. While the prevalence in Israel used to be 100 cases per year, it dropped to 40 per year (despite increase in deliveries). This reduction is predominantly attributed to education of the population to avoid risk factors such as prone position, excess clothing, over-heating, soft mattress, smoking and bed sharing. The usage of pacifier may also reduce the risk of SIDS (2,3).
The pathophysiology of SIDS is still unknown and most probably does not represent one disease but rather a combination of various factors including respiratory control immaturity, arrhythmias, brainstem/pons abnormalities, and potentially yet undefined factors (1, 4-10). Due to the unclear pathophysiology and etiology, along the importance of understanding respiratory maturation and infants’ breathing patterns, and evidence of previous apneas in victims of SIDS, a trend of monitoring infants’ respiration have been emerged (11-25). Although the literature is not completely decisive of monitor usage to prevent SIDS, these are definitely recommended in high risk infants. Although the reduction in the prevalence of SIDS is justifiably attributed to the “back to sleep” campaign, it is plausible that the ongoing increase in home alarm-monitors contributes as well to this observed reduction of SIDS. From our clinical experience, not negligible amount of infants were brought for assessment due to alarms of the Babysense they used in their home, and were found to have immature respiratory control.
Several studies have assessed the relevance of cardiorespiratory monitoring in high risk infants and some have reported that such monitoring can identify apneas early and potentially prevent death (15, 26). However, while direct monitoring of respiration and heart rate requires attaching surface electrodes to the infant, movement sensors may be placed under the mattress and detect respiratory cessations without touching the infant, since infants’ breaths are associated with movements. Thus, we have planned the current study to compare between alarms of a cardirespiratory recorder with that of under the mattress sensor recorder. We hypothesized that both monitors will be accurate in alarming in cases of apneas.
Methods
54 consecutive high risk infants who presented to the emergency room with Apparent Life Threatening Event (ALTE) underwent a whole night simultaneous monitoring by both cardiorespiratory monitor (intellivue MP20 junior, Phillips) and under the mattress movement monitor (Babysense II, Hisense). The cardiorespiratory monitor was set to alarm when detecting no respiration for 20sec, heart rate below 90/min, and oxygen saturation below 90%. The Babysense was set to alarm when detecting no respiration (movement) for 20sec. The study was approved by the Rambam Medical Center IRB for studies in humans, and parents’ of the infants have signed an informed consent prior to participation. Inclusion criteria consisted of all high risk infants who were admitted to the hospital, in ages below 1 year (e.g. infants with apparent life threatening event (ALTE), infants with Babysense alarms in their home). There were no specific exclusion criteria.
Intellivue MP20 junior, Phillips
The Intellivue MP20 monitor (Phillips Electronics, Eindhoven, Netherlands) is a portable monitor with various functions which can be individualized and fit to the patients (Fig !). In the current study 3 channels were recorded and utilized: Heart rate (driven from 2 specific chest ECG electrodes attached to the studied infant), respiratory rate (driven from the same electrodes), and oxygen saturation (driven from a sensor placed on one of the studied infants’ fingers). The monitor was connected to the infant throughout the study in parallel to the Babysense recorder (see below), and was set to alarm when specific threshold were crossed (no respiration for 20sec, heart rate below 90/min, and oxygen saturation below 90%).

Fig 1: Intellivue MP20 junior, Phillips Electronics, Eindhoven, Netherlands.
Babysense recorder
The BabySense monitor (Hisense health monitor technologies, Rishon Le Zion, Israel) is an ambulatory infant monitor which detects respiration by movement sensors placed under the mattress of the studied infant (Fig 2). These are two highly sensitive sensor pads which detect micro movements through the mattress and was set to alarm when the were cessation of respiratory movements for 20sec.

Fig 2: The BabySense monitor, Hisense Health Monitoring Technologies, Rishon Le Zion, Israel
Study data collection:
The following parameters were recorded in the study:
Demographic parameters (age, gender, gestational age at birth, parental smoking), diagnoses (such as ALTE, Bordetela Pertusis, Respiratory Syncitial Virus, gastro esophageal reflux, respiratory control immaturity), medical treatment (respiratory stimulants such as methylxantines, antibiotics, oxygen, H2-blockers), and a detailed nocturnal event log (i.e. time of any alarm by any of the recorders, and manual measurement of heart rate and oxygen saturation at the time of the alarm (by the nurse is shift).
Statistical analysis
All events were recorded and a chi-square test for proportions was used to compare the alarms of the two recorders. P<0.05 was considered to be significant.
Results
Fifty four infants (aged 47±40 days) who presented to Rambam (n=49) or Carmel (n=5) emergency rooms after ALTE participated. Alltogether, there were 80 nights of monitoring (18 infants were monitored for 2 nights, 4 infants were monitored for 3 nights). During these nights, alarm was noted in 8 nights. The demographic and monitored parameters of those with alars and without alarms, and for the whole cohort are presented in table 1. There were no statistically significant differences between the alarming and non-alarming infants with regard to age, gestational age, weight, birthweight, gender, fever or oxygen saturation upon admission. Heart rate at rest was lower in alarming infants compared to non-alarming infants (145± 11 vs 161± 19, o=0.05). While alarming, both heart rate and oxygen saturation were marked and were significantly lower (82± 9 BPM and 77± 9%, respectively). Overall there were 8 events of alarming (10%), in all cases simultaneously in both monitoring systems. In all other cases there were no alarms in both systems. These results are shown in table 2.
Conclusions
Under the mattress movement sensing is accurate in alarming for apnea and bradycardia in infants. Since the usage of this system is simple and without direc
- Always put a baby to sleep on its back. (This includes naps.) DO NOT put a baby to sleep on its stomach. Side sleeping is unstable and should also be avoided. Allowing the baby to roll around on its tummy while awake can prevent a flat spot (due to sleeping in one position) from forming on the back of the head.
- Only put babies to sleep in a crib. NEVER allow the baby to sleep in bed with other children or adults, and do NOT put them to sleep on surfaces other than cribs, like a sofa..
- Let babies sleep in the same room (NOT the same bed) as parents. If possible, babies cribs should be placed in the parents’ bedroom to allow for night-time feeding.
- Avoid soft bedding materials. Babies should be placed on a firm, tight-fitting crib mattress with no comforter. Use a light sheet to cover the baby. Do not use pillows, comforters, or quilts.
- Make sure the room temperature is not too hot. The room temperature should be comfortable for a lightly-clothed adult. A baby should not be hot to the touch.
- Offer the baby a pacifier when going to sleep. Pacifiers at naptime and bedtime can reduce the risk of SIDS. Doctors think that a pacifier might allow the airway to open more, or prevent the baby from falling into a deep sleep. A baby that wakes up more easily may automatically move out of a dangerous position. If the baby is breastfeeding, it is best to wait until 1 month before offering a pacifier, so that it doesn’t interfere with breastfeeding. Do not force a baby to use a pacifier.
- Keep your baby in a smoke-free environment.
- Breastfeed your baby, if possible – breastfeeding reduces some upper respiratory infections that may influence the development of SIDS.
- NEVER give honey to a child less than 1 year old – honey in very young children may cause infant botulism, which may be associated with SIDS.
Use Babysense Breathing Movement Monitor.
Technical Specification
- Requires 4 AA Alkaline Batteries (not supplied)
- Sensitivity setting – Pre-set
- Power consumption approx. 1mA
- Battery life approx. 6 months using high quality alkaline batteries
- Alarm volume typically 85dB SPL at distance of one meter from control unit
- Illumination typically 2mCD
SIDS – Sudden Infant Death Syndrome
SIDS is the unexpected, sudden death of a healthy baby under age 1 in which an autopsy does not show an explainable cause of death.
SIDS remains the leading cause of death in infants under one year old in most countries throughout the world.
With an average 5 out of every 10,000 death rate, SIDS death toll reaches 5600 babies per year in the USA and Europe alone.
SIDS is impossible to predict and modern medicine has not yet come up with means of care or solution.
Causes, incidence and risk factors
The cause of SIDS is unknown, although there are several theories. Many doctors and researchers now believe that SIDS is not a single condition that is always caused by the same medical problems, but infant death caused by several different factors.
These factors may include problems with sleep arousal or an inability to sense a build-up of carbon dioxide in the blood. Almost all SIDS deaths occur without any warning or symptoms when the infant is thought to be sleeping.
SIDS is most likely to occur between 2 and 4 months of age, and 90% occur by 6 months of age. It occurs more often in winter months, with the peak in January.
SIDS – Symptoms
There are no symptoms. Babies who die of SIDS do not appear to suffer or struggle.
SIDS – Signs and tests
Autopsy results are not able to confirm a cause of death, but may help add to the existing knowledge about SIDS.
The following have been linked to an increased risk of SIDS:
- Babies who sleep on their stomachs
- Babies who are around cigarette smoke while in the womb or after being born
- Babies who sleep in the same bed as their parents
- Babies who have soft bedding in the crib
- Multiple birth babies (being a twin, triplet, etc.)
- Premature babies
- Babies who have a brother or sister who had SIDS
- Mothers who smoke or use illegal drugs
- Teen mothers
- Short time period between pregnancies
- Late or no prenatal care
FAQ
Babysense breathing movement monitor does not replace parent or caregiver. It is an attention-calling device, a parent’s or caregiver’s aid. It cannot solve all problems, it cannot actively take action. It can only call our attention if it registers a respiratory distress. This may provide critical time to intervene.
Babysense breathing monitor cannot replace or substitute the important safety guidelines every parent should observe regarding an infant’s sleeping conditions: Sleeping on the back, never overheating the room, never smoking around the child, firm bedding materials and taking caution with blankets and suffocating hazards. Additionally, every parent and caretaker should be familiar with basic first aid, to enable optimal and prompt action in case of need. Observing these safety guidelines, together with using a Babysense respiratory movement monitor, will optimize your child’s safety and enable you both peace of mind and a good night’s rest.
Operating tips
- To avoid possible danger of strangulation from cords, keep the cords out of reach of children. Ensure that excess cords are secured with the included cable tie.
- Always insert 4 AA NEW alkaline batteries.
- When monitor is in use, do not attach crib mobile or other moving toy to infant’s bed/crib/cot (they can easily be mounted on the wall over the crib).
- Do not put any additional infant or pet in the bed.
- Keep the sensor pads away from source of heat.
- Bed base should be rigid (plywood) to ensure the sensor pad and the mattress are tightly pressed together.
- When not in use over long periods, always remove batteries from the device and store in a dry shaded place..














